At least eleven states, including Wisconsin, have sought approval from the United States Department of Health and Human Services to require work or some form of “community engagement” to maintain Medicaid eligibility. These proposals have been the subject of controversy and debate regarding their goals and anticipated effects.
Proponents and opponents of Medicaid work requirements generally agree that work is beneficial to people’s economic, mental, and physical well-being. There is plenty of evidence to support this view. Unsurprisingly, people who are employed at higher paying jobs receive more of the economic benefits of work, including the ability to afford health insurance and medical care.
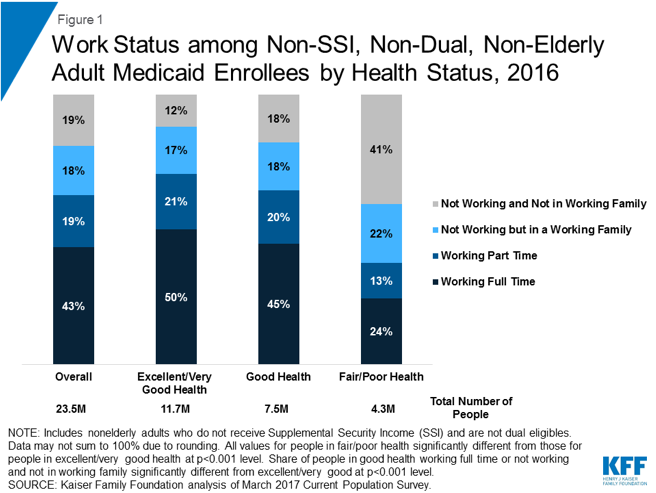
Proponents of work requirements argue that there are people receiving health insurance coverage through state Medicaid programs that could be working but are choosing not to. Conditioning Medicaid coverage on a work or community service requirement will therefore motivate people to participate in the workforce and presumably secure health insurance coverage other than Medicaid.
Opponents note that the majority of able-bodied adults enrolled in Medicaid are already working, often at low-wage or part-time jobs that do not offer health insurance. Adults enrolled in Medicaid who are not working are most typically either unable to work due to illness or disability, or have caregiving responsibilities, all of which would qualify these individuals for exemptions from most states’ proposed work requirements. Thus, the argument goes, imposing work requirements would do little to advance the stated goals of the advocates of these requirements, while the combination of work requirements themselves and burdensome administrative documentation requirements would cause many people to simply lose health insurance coverage without a net improvement on participation in the workforce
Medicaid Work Requirements Likely to Cause People to Lose Eligibility
The Kaiser Family Foundation recently estimated that between 1.4 and 4 million beneficiaries could lose Medicaid coverage nationwide if work requirements were implemented in every state. These projections are tied to a combination of people who would be assumed to fail to meet reporting requirements or would not meet the work requirement altogether. In the first month that the Arkansas Medicaid work requirement was in effect, for example, 445 people met the work requirements. More than 7,000 of the 18,000 people covered by the requirement did not meet it and are now at risk of losing their coverage if they fail to meet work requirements for a second consecutive month.
Are Work Requirements Consistent with Medicaid’s Purpose?
The effects that have been seen in the early days of the Arkansas work requirement implementation are exactly what caused the federal courts to invalidate Kentucky’s work and community engagement requirement earlier this summer.
In overturning DHHS’s approval of the Kentucky requirement, the court found that by increasing premiums and imposing work, community service, and administrative reporting requirements, Kentucky’s community engagement requirement would likely result in loss of eligibility for many people on Medicaid, particularly the populations made newly eligible by the Affordable Care Act. The court therefore found that the Kentucky approach was inconsistent with the basic objectives of the Medicaid program, which are to furnish medical assistance to people without the necessary means to meet the “costs of necessary medical services” and rehabilitation and other services to help “families and individuals” achieve or maintain “capability for independence or self-care.” (42 U.SC. § 1396-1).
At the end of the day, the court concluded that DHHS did not have the authority to constrain the Medicaid program in ways that were likely to close the front door of eligibility, even if the apparently intended result was to improve health and well-being by promoting work.
Benefit Cliffs and Political Risk Ahead?
The Washington Post observed that even if other states survive a legal challenge to their work requirements where Kentucky so far has not, and even if current Medicaid enrollees meet all work and other administrative requirements, work requirements may still push people into a coverage gap. People who manage to comply with work requirements may end up earning too much income to qualify for Medicaid in states where Medicaid eligibility is below 100% of the Federal Poverty Level, while not earning enough to afford coverage in the ACA insurance exchanges or having the opportunity to elect employer-sponsored health insurance.
No state legislator or governor standing for reelection this fall is eager to see the ranks of the uninsured grow on his or her watch. The desire to pair public benefits with work, community service, drug testing, and other tests will be evaluated by voters against the growing public sentiment that the United States, and the states individually, must find a way to provide basic health care access, especially for those with common chronic diseases or other pre-existing health conditions, for all.